The Brian Allman
Diffuse Large B Cell Lymphoma Novel Therapeutics Program
Brian Allman: Notes of my Battle with Cancer
Intro
Post - May 2022
I have had Non Hodgkins Large B-cell Lymphoma (DLBCL) for over two years. I am otherwise,a healthy 65 year old male and I regularly exercise riding my road bike three to four times a week for 90-150 minutes each time. I ate well, no fast foods. When I discovered my cancer, it came on very quickly and within a 10 day period went from the point of noticing something might be wrong to having a 19cm tumor in my abdomen (um, that's the size of a volleyball) which I must say made me look like I was eight months pregnant. I have pictures and given the amazing growth of this tumor I'm sharing here. While I was scared to death about it, I also had to laugh at my newly-formed physique!
I live in Los Angeles and was fortunate enough to go to Providence St. John's in Santa Monica and they were terrific. That's where I met my first oncologist Dr. Kristeja who took amazing care of me. I used to tell him he saved my life and that I'm a big fan of his. This is where I went through my first Chemo treatments in 2019 when six different therapeutics were infused in one day every third week.
First Line R-CHOP
This first line of treatment was with R-CHOP, a combination of (R) rituximab, which is not a chemotherapy drug but is composed of man-made antibodies that help your immune cells destroy cancerous tumors; (C) Cyclophosphamide, a cancer drug; (H) Doxorubicin hydrochloride, a cancer drug; Vincristine (older name: Oncovin), a chemotherapy drug that slows or stops cancer cells from growing; and (P) Prednisone. It's a first-line treatment for aggressive non-Hodgkin's lymphoma.
The three months of treatment put me into remission and caused huge elation. However, the remission only lasted less than 60 days. In all honesty, I found this shocking, not really understanding how cancer and the treatment of it truly works — or in many cases doesn't!
Photos with my doctors during various treatments

First line treatment - R-CHOP Infusions with Dr. K
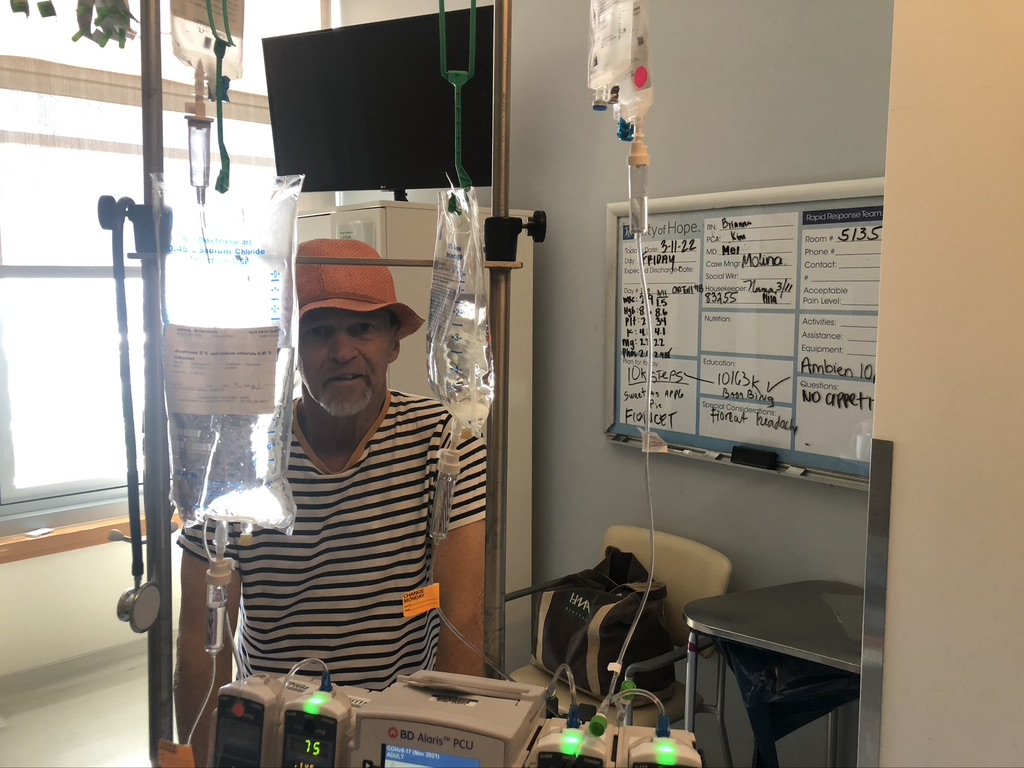

Showing off my new physique with a volleyball-size tumor in my abdomen.
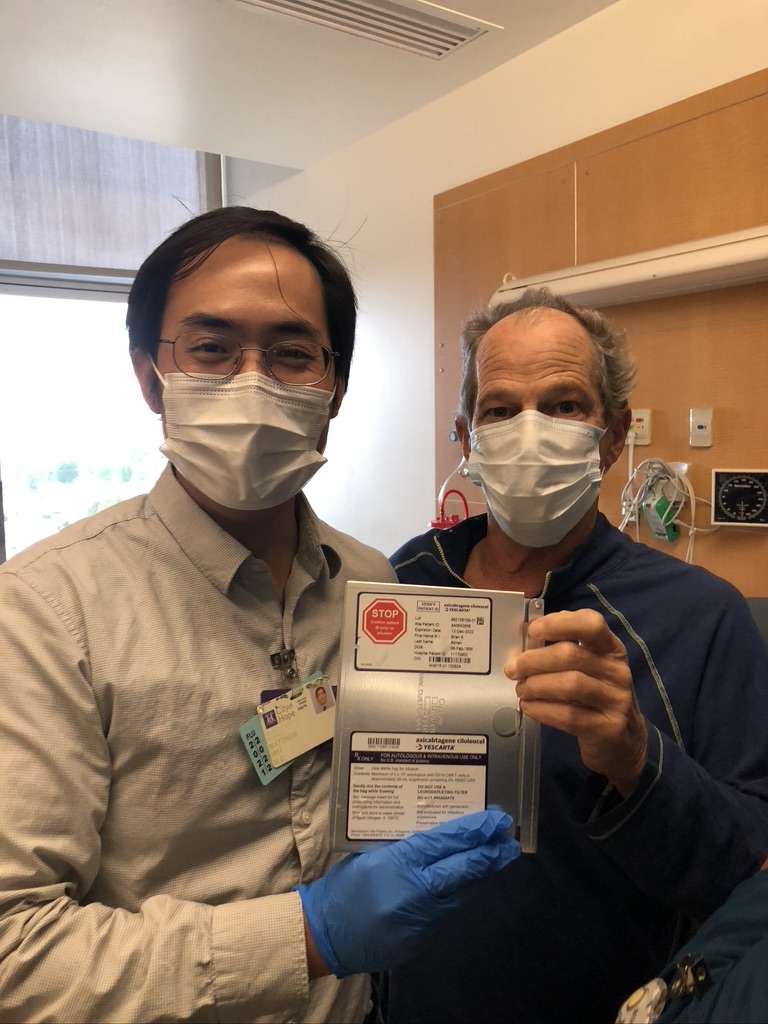
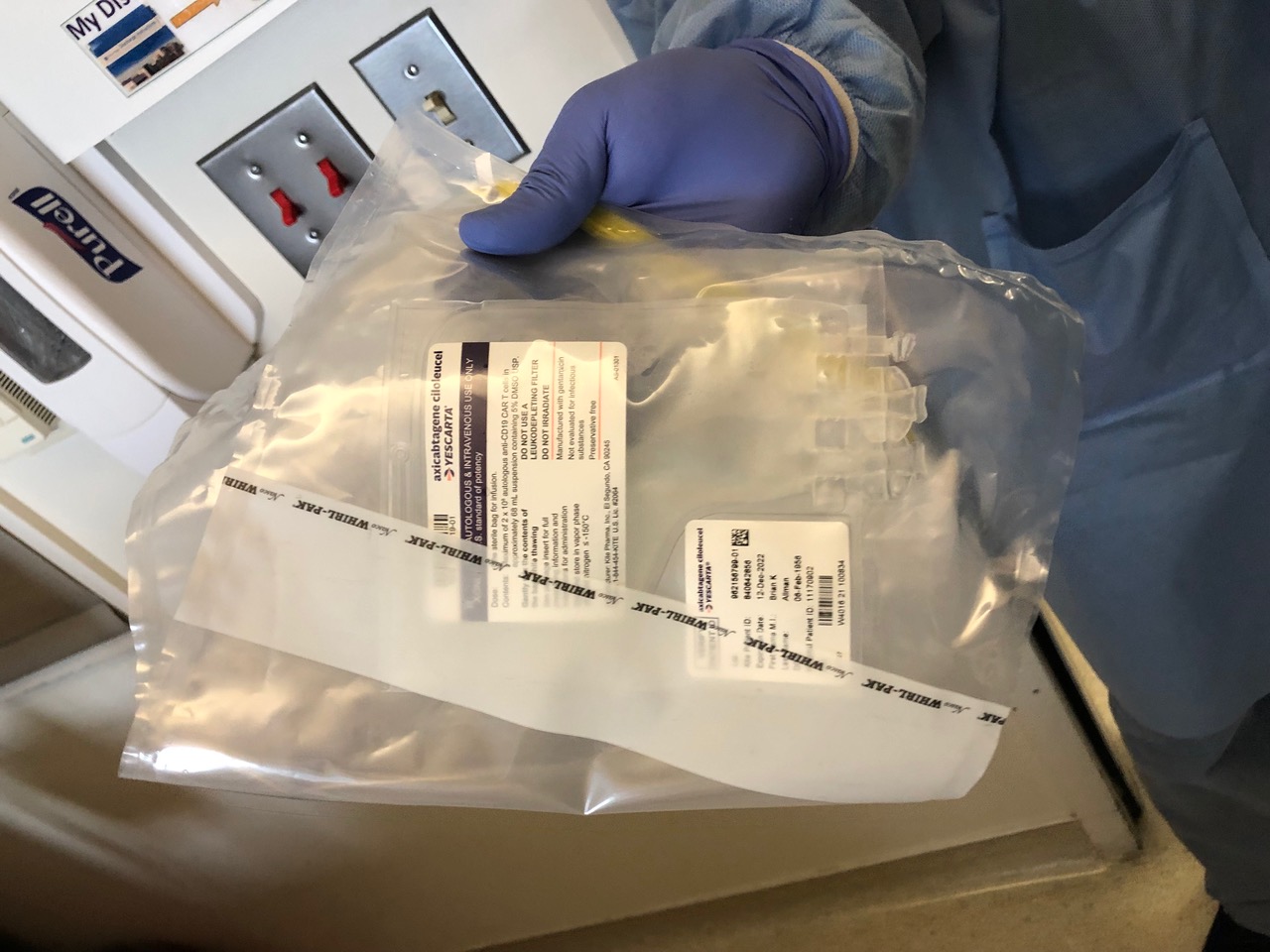
Dr. Mei at City of Hope and the Car T-cell package "Brrrr, -150°C (- 240°F)."
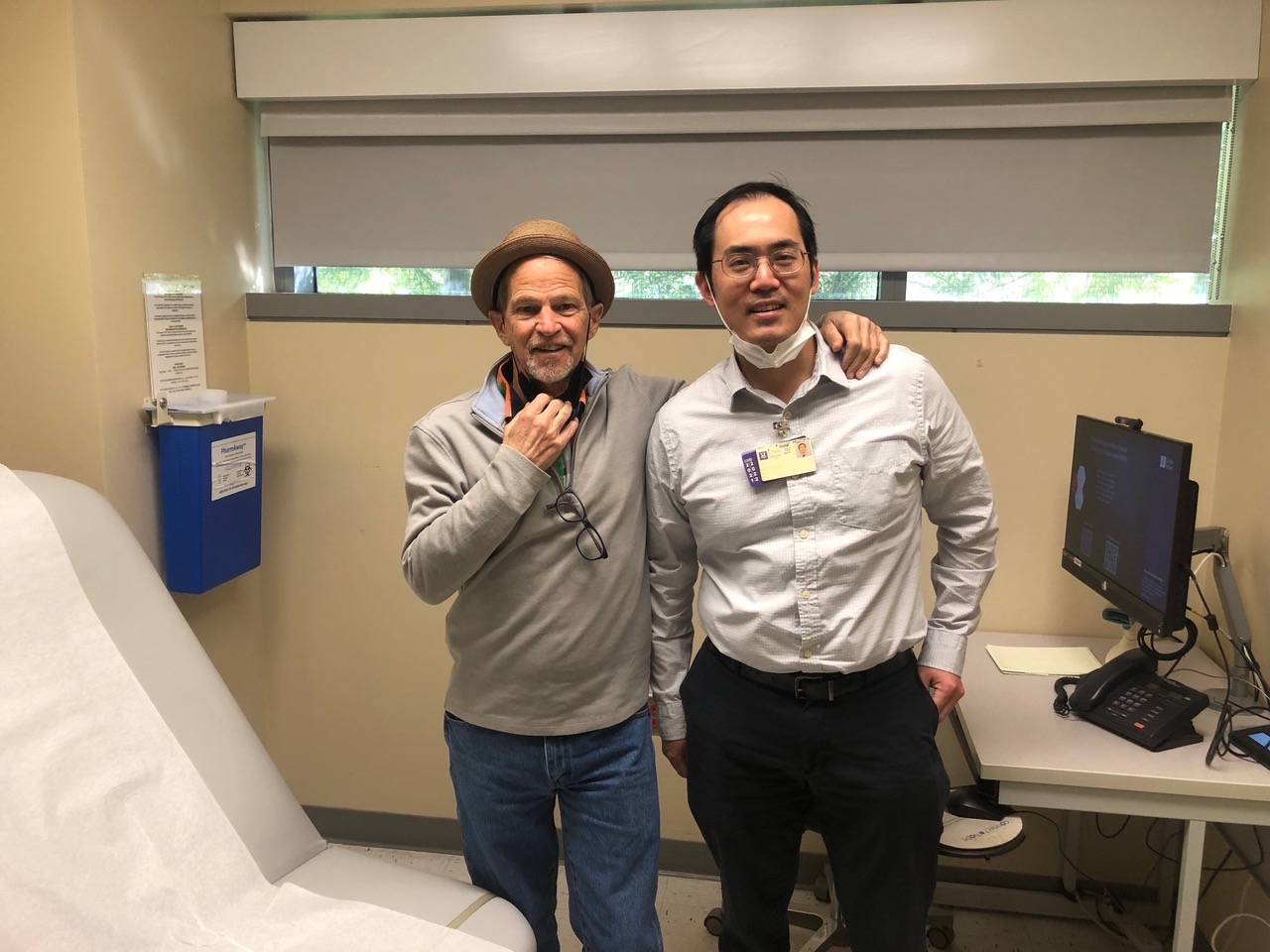
During my time with Dr. K at St. John's I learned that he had done a fellowship at City of Hope and I was fortunate enough to have Dr. K introduce me to my current doctor, Mathew Mei, M.D., Hematologist - Oncologist. Dr. Mei is involved in some clinical trials and I became an ideal patient for one of his studies with Polatuzumab.
Let me say up front, City of Hope is an amazing place— a cancer-only hospital with some of the best minds in the field of cancer doing studies and research and luckily for me, in the Los Angeles area. I cannot give them enough credit for what they do and Dr. Mei is my current hero.
Polatuzumab
The Polatuzumab treatments were a bit tougher than my previous Chemo treatments. The infusions were also every third week however it was for three continuous days. Day one was being in the chair for 10 - 12 hours, then six or seven hours on day two, and four to six hours on day three. City of Hope has a program with on-site housing so I stayed there the three days of infusions. This was amazing because otherwise, it would have been expensive to stay at a hotel for all that time.
The 12-hour days were brutal and took a lot of mental and physical engergy just to get through the days. The side effects were perhaps not as bad as the R-CHOP but realistically, I was beat up and the fatigue was always present. Some days I just knew that I would be in bed or on the couch most of the day. Some days, when I got up to go to the kitchen, well that was all the physical movement I could do.
I'm a very active person and the fatigue really bothered me; admitting I was just too weak to do more meant having someone around for those first few days coming home from the treatments.
Stem Cell Transplant
Bone Marrow Stem Cell transplant. Well, after the Polatuzamab proved not to be the answer to my cancer when it came back after just five or six weeks, it was decided that my best option was for an autologous stem cell transplant. I was quite happy knowing many people have seen very positive results doing this and I got myself mentally prepared for it.
City of Hope has a great record and reputation for these transplants and I could not have felt better with my fortune to be at this hospital with these world class doctors and staff and they were simply as good as it gets.
I started the process as soon as they could get me in there, perhaps a week after realizing my cancer had returned so quickly and aggressively. First, I got a Hickman port, a life saver in the process of infusions, and they got me ready for the transplant process which is very much like you've seen with dialysis. The floor where this is done is well set up, comfortable, because when you do the process, called aphersis, you are stuck in that room. It is a special machine and you cannot move it around for things like bathroom breaks. The process generally takes four to eight hours per day to harvest your cells. Most people can harvest enough stem cells in three or four days.
Unfortunately, my stem cell production was not doing what it was supposed to and when we reached day five of my harvesting we were not even half way with enough cells. In all honesty, I was disappointed in myself, kind of like not being able to perform in a physical contest, and that threw me mentally. My doctor decided to keep going and we did another two days to see if I could get enough to try the transplant. I think you need about two million of your cells and after seven days we had less then a million, I was a failure at producing my own cells.
My doctor was awesome through all this, and the staff at CoH could not have been better or more supportive, so we decided to take two weeks off and let my body heal and then come back and try again. This was not a popular decision with the staff that deals with this every day but they understood and we forged forward to see if we could produce the positive results in two weeks. Well, I did another two days and the stem cell numbers just would not reach our goal. Apparently, chemo treatments affect your ability to produce these cells and well... I guess mine were affected negatively so I could not come in first in the stem cell race.
So, what next doctor?
My doctor decided, with his transplant team, that I was a good candidate for CAR T-cell treatment. With some time to get my strength back from the Stem Cell debacle we set a date of December 22 to start the process. Oh, what a Christmas present this would be. And then, I got COVID!
CAR T-cell therapy
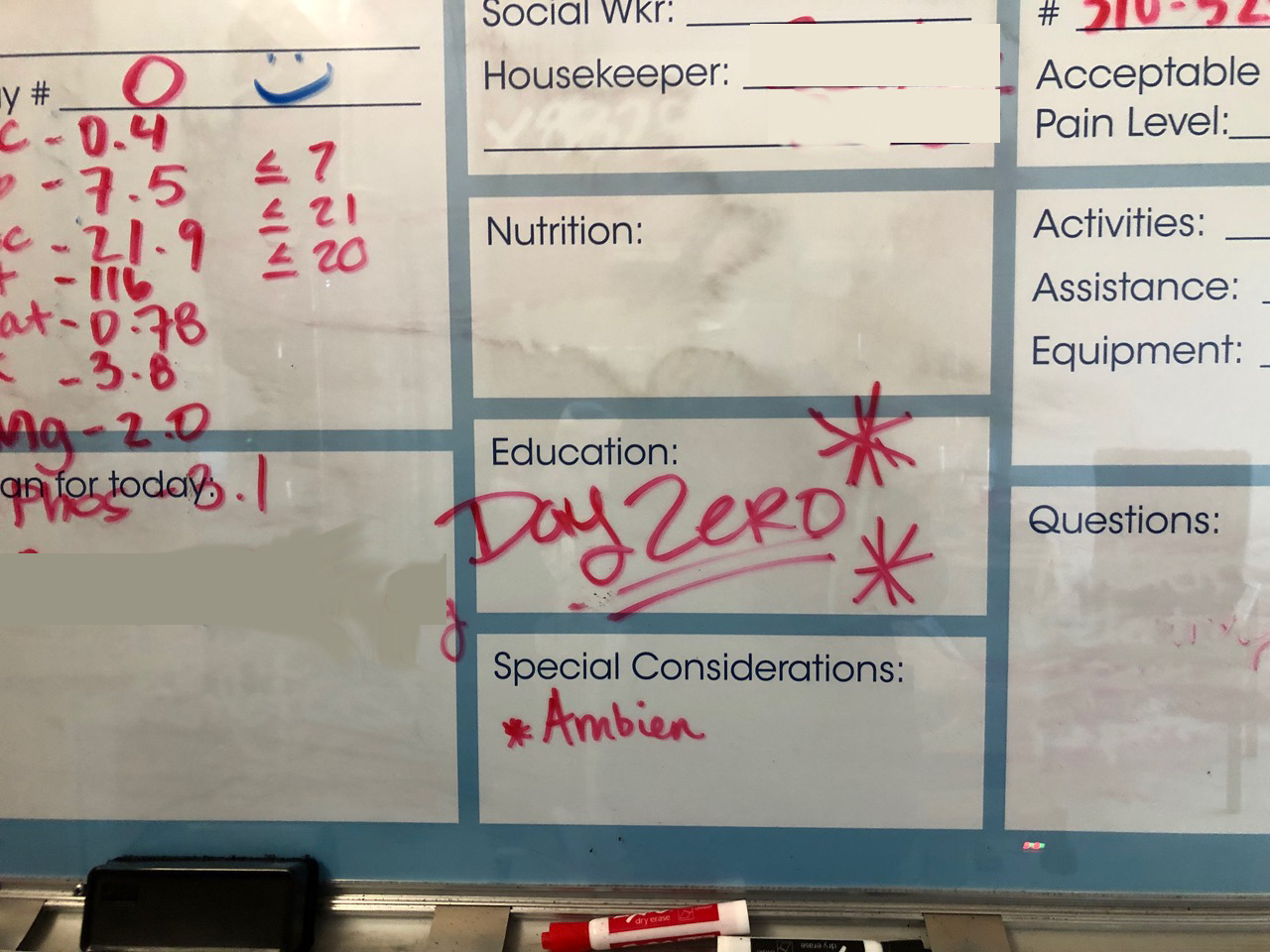
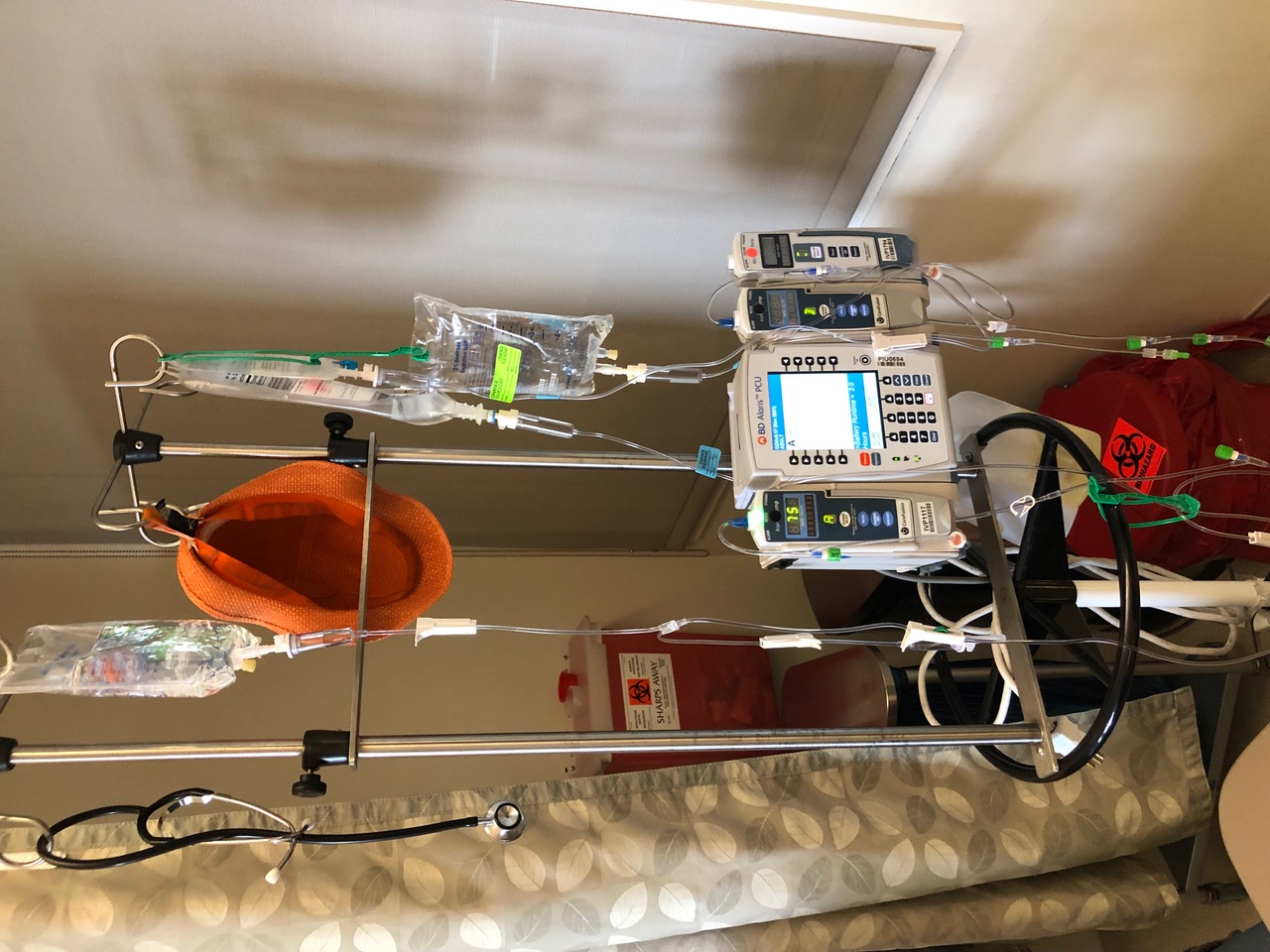
Well, yesterday was quite the amazing day, it's what they call Day Zero or your CAR T-cell birthday when they infuse you with the genetically engineered cells. There are many months leading up to this day and I wanted to, and did, make it very special and ceremonial moment with all the people who who were present. I asked my doctor to be there when it happened. Apparently this is not common but I wanted to share this moment with him and I am glad that I did.
The guy that brought me the cells... they called him the scientist because they deliver the cells in a special box that has a frozen environment at 150 minus degree temp, which I thought was really cool. He got excited because I took pics of that device that he used to deliver the cells. I made him take a pic with me and then he gave me the device that the infusion package was delivered in. I don't think this is common practice but it certainly added to the excitement of the moment.
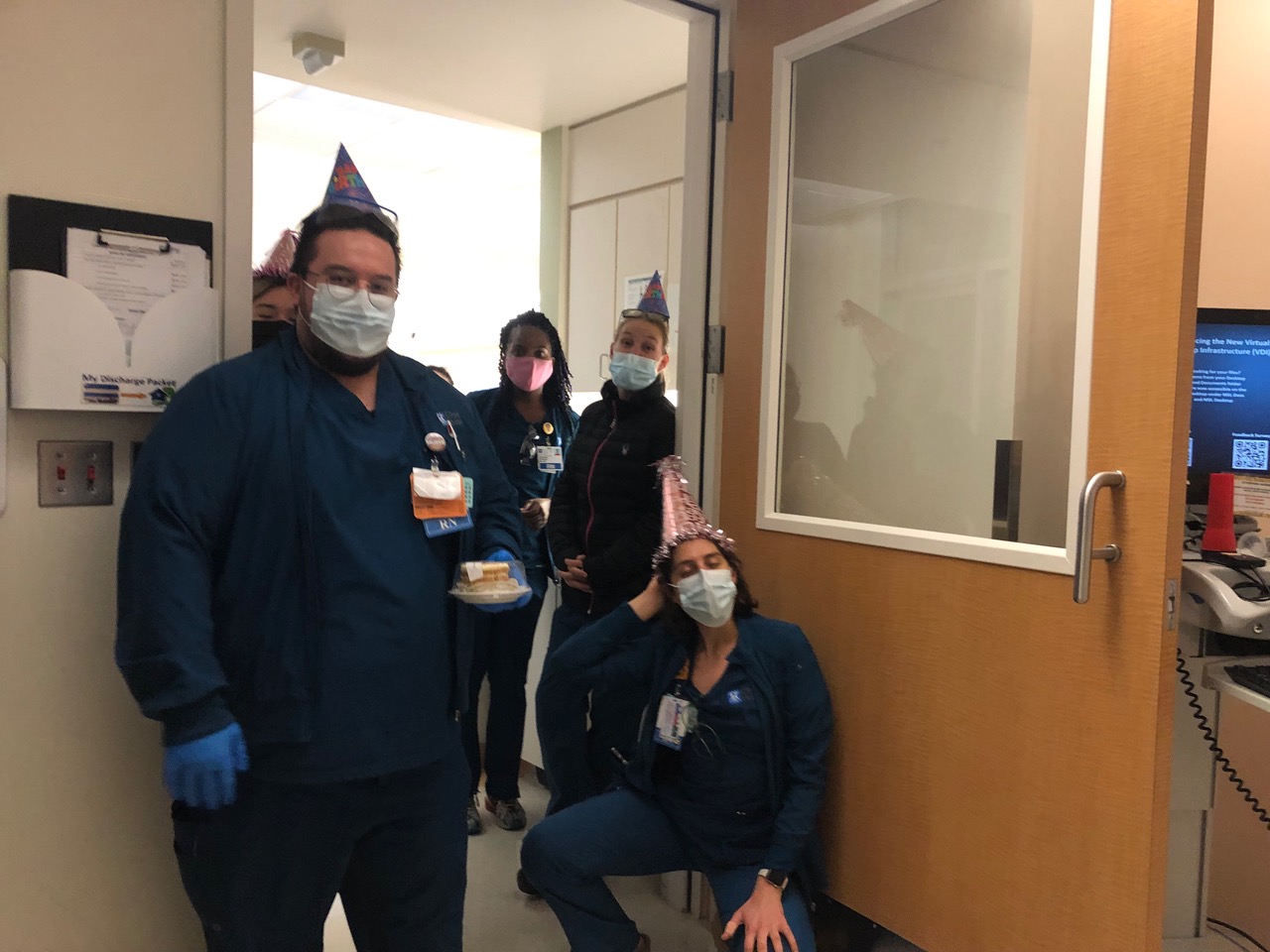
I think there were six hospital people there so my room was full, and it made the moment bigger which I now know helped me with the moment. So we did the infusion and in reality I felt nothing. But hours later I found myself super fatigued, lying on my bed. I'm not that guy. I normally would try to exercise to feel stronger and I slept off and on for four to five hours. I thought it was a physical thing happening. But now today, in reflection, I'm realizing that it was just a huge emotional reaction after months of building up to this one moment that I believe is going to be my cure to my cancer. Oh, and at about 8 p.m. the entire floor nursing staff came to my room and sang Happy Birthday which was emotional and I can't thank them enough for what they do.
Then I woke up today (Day 1) feeling pretty damn good, and I started to share with a few people the comment, "I'm different today then I was yesterday… no really, I am genetically not the same person I was yesterday and how many people can say that and it's actually true." I'm making light of this but it feels good to say, my DNA is different today then yesterday, and it makes describing what was actually done a bit easier to talk about.
I wrote the above in the early days of the transplant and wow did I have no idea just what I was in for. While I was quite nervous about how it might affect me cognitively, I really hadn't thought much about the physical implications. All that I read didn't set me up for what was about to come at me: 10 days of serious fever which set off a lot of other physical ramifications but I was absolutely bed ridden for 10 days, just feverish 24 hours a day, sweating, chills, fatigue so I was unable to go to the bathroom by myself and my respiratory issue was very scary and not unsimilar to how I felt during my time in the hospital with Covid. In short, it knocked me on my ass and took a lot of attention from the doctors and a lot of medications just to address the symptoms along with what the needs were for the T-cell transplant.
I can say it now, I was overwhelmed by it, definitely not prepared for it mentally and I was not able to combat it as I normally would through exercise on a daily basis. I literally couldn't get out of bed to walk 10 steps, much less 10k. My physically weak reality took over my ability to be as positive as I normally am and that's a lesson we all need to address,. When you least expect it you need that inner strength, that voice that tells you "Yes, you can do it, You can overcome all these unseen obstacles and once you tap that, well Cancer and it's ailments can just take a back seat."
Gear up before you do these treatments.It is your job to be ready for whatever comes your way. There are not enough medications to do this alone so I strongly urge anyone facing this to start their own reality check as to how they might handle things when they just are not as we thought they might be. Also, I want to add that I was so very concerned about how the CAR T-cell would affect me mentally (they warn you about the cognitive affects and they do cognitive testing on you four times a day). But the thing was, I had no affects mentally. It was the physical and well, as I've said, it really threw me.
From the CAR T-cell therapy I was in the hospital 33 days, three for Chemo, two prep, CAR T-cell birthday (I have pics of the hospital staff and they were awesome), and 28 days in observation/recovery. Believe it or not, I was so fatigued and physically weak I wasn't sure I was ready to go home. Imagine that long of a hospital stay and think you might need to stay longer.
"Oy!" I said. But home I went.
Recovery has been slower than I expected. I had a respiratory issue which stopped me from doing any exercise, even walking, as I would be seriously out of breath within just a couple of steps. I felt tired a lot and took many naps a day.
The breathing problem took about two weeks to begin to subside and the fatigue lasted several weeks longer.
February 2023 Report
My Notes From October 2022 to February 2023
It's time to report out what my last eight-plus months have been like as they have been full of cancer treatments and other surprises like COVID-19 and tuberculosis! That's right. After my failed stem cell attempt, treatments of Imbruvica, Polatuzumab vedotin, IMB2323, and a very serious bout with COVID-19 which had me hospitalized for 10 days in quarantine.
I received monoclonal antibodies and Remdesivir. Yikes! Then a Car-T cell transplant kicked my butt with side effects. (Do you know about Cytokine Release Syndrome? You need to be checked three times a day for cognitive competence.) It still did not work on my cancer.
I took bridging steroids to get me along without having any chemo and then I got Tuberculosis. What? How?
A lesion was found on my lung which caused the doctors to do a biopsy that revealed I had somehow contracted TB. I still cannot believe this. I mean really, what else might they throw at me/us? I still wonder, "How did this happen?" My best guess is that I contracted it at a hospital.
With the TB, I was very sick at home and then started acting very confused, saying weird nonsensical things, and sleeping all the time. My wife knew something was seriously wrong. She eventually had to call an ambulance to come get me. I have zero recollection of the ambulance incident. I was down and out in a local Palm Springs hospital where they quarantined me and then discovered the TB—thank you very much.
While I was quarantined, hazmat suits were required for anyone coming into my double-door access hospital room. It was very scary and lonely. It took many days to uncover the TB and decide what to do with me.
At this point, I just wanted to be transferred to my cancer hospital, City of Hope, where my hero cancer doctor resides. But because I was under quarantine I was not allowed to be moved or see anyone for days on end. All I remember from that time was the tiny window that I could look out but only into the little anti-room where the attendees prepared to come into my room in their safety suits.
My wife, bless her, would bring me some food (that I was unable to eat) and wave through the two rooms so I could see her. This became the highlight of my days. The appetite loss started me on a path of severe weight loss that I am only now addressing. I just couldn't eat and when I did eat, I was unable to taste it. Is this a result of Long Covid? No one knows. I got down to 113 pounds from somewhere in the 145-150 range and I did not look good!
Upon returning to our home, I had to again be quarantined for another 10 days—as if I wasn't crazy enough! TB is serious business and as an infectious disease, is overseen by the government. So, I was not being directed by doctors that I had chosen but by the government-run Infectious Disease Team. They have strict protocols for the quarantine as well as the serious antibiotics you have to take continuously for a year. I worry about these medications and how they will affect my organs in the long term however I continue to take them now.
Oh, I forgot something. While taking the Imbruvica I developed a serious rash. I mean I was covered head to toe with this very ugly rash that itched like nothing I had ever had before. It added more insanity to my daily process with this scratching, I was a mess. I might have pictures because it was really something to see.
Also, when I was going through my bout with Covid, it was exhausting leaving virtually no energy to do anything. I've never been fatigued like that and they just didn't know if the drugs they were giving me for coronavirus (Remdesivir) were working against the chemo medications but I literally was unable to stand on my own and talking took just too much energy with my reduced breathing capacity.
As a result, I became secluded, not wanting to talk to any of my family or support team or friends because it took too much energy and left me depleted emotionally. It was a serious mistake to cut off communications and not cozy up to them for their support. I needed them and it was a serious life lesson to learn I needed to absorb and ask for the strength of others. Seclusion is not a positive thing for an illness, at least not for me.
Despite all these battles and setbacks, I did just find out that my TB is gone. (Did I ever really have it?) I have what they call MAC lung disease which is not as serious as TB but there is still the same need to keep any disease from coming back, so the antibiotic medications continue. Because of the TB, they had to stop all my cancer treatments and this left my cancer unattended for about eight weeks.
Backtracking just a bit, when a lung lesion was found a biopsy was done and my City of Hope doctor saw a new or specific marker that he realized might work with the drug Keytruda. We started that process once my strength started to come back. I am on my fifth dose of Keytruda and after a PT scan last week it is showing NED (no evidence of disease).
How did that happen and how long will it last? I have so many emotions from this both positive news – "Yippee I'm cancer free!" to questioning, "Am I?" However, my doctor does not know how long we will keep up this treatment or if or when the cancer might return.
It's pretty amazing that I am able to exercise by walking 6000 to 10,000 steps per day. I've also found a fitness class being taught in the park where I walk, so I'm participating in this too and am headstrong to get my strength back. I'm still fatigued but working on this path back to a strong body, and mind, to fight anything else that comes my way.
One last thought about my current condition now that I have no evidence of disease. Finally, after more than two years of dealing with my cancer 24/7, I have a new task at hand. The complicated history I've had dealing with my illness has prevented me from being involved in anything other than doctors, and hospitals, and just getting through the day. I think my brain has atrophied and in short, I've become boring.
I can't seem to remember anything and I'm physically exhausted all the time so I'm finding it difficult to concentrate and engage in interesting conversation. Additionally, for these last few years, I've only had one purpose: to do whatever I can to heal. However, now I find myself just unsure of what my daily or long-term purpose in life really is and I find that very disconcerting.
I used to have full days of work, cycling, networking and seeing friends and family. Currently, having moved to a new city (Palm Springs), I seem to have none of these and am unable to answer what drives me forward on a daily basis. I ask, "How can I get back to being a contributor to the community?"
It's only been weeks since I am able to go out into the world again, to be around people (masked of course) and offer up time to get involved. I'm not complaining but just acknowledging that I perhaps could have prepared for this day much better. It's imperative that I find myself again and I've started that process but it's slow going so far.
This is a challenge that I had never thought about before now but I am certainly addressing it and you should know this; recovering from an illness is also a challenge and you might not be able to prepare for it even if you are forewarned.
January 2024 Update
I am currently a DLBCL survivor. I'm thriving physically and it can happen for you too.
I went through three years of many different treatments and with a variety of medical complications. I started my journey with a typical Chemo cocktail treatment R-CHOP, which worked for about a month. I thought my cancer was over in those first few weeks (silly me). However, what I had no idea of, was the journey ahead that I would be on to find the right treatment for me.
I was diagnosed at the St John’s Hospital in Santa Monica, California by a doctor who I am still in touch with. When the first treatment did not work and the cancer relapsed so very quickly my doctor knew it needed special attention and he referred me to my current hero, Dr. Matthew Mei, at the world’s best hospital City of Hope in Duarte CA. City of Hope specializes only in Cancer and they saved my life. It was not an easy path to my current remission but Dr. Mei was steadfast in his determination to help me get well. Having Dr. Mei as my doctor is why I am able to share this message with you.
There are advancements in cancer research daily and keeping up with it must not be easy for doctors given their patient loads. When a treatment failed (and they did) Mei was already thinking ahead, sharing information and collaborating with his team to understand what next might be best for me. Having a hematologist/oncologist who you trust, one that you can challenge and share in the most minute of details is essential in finding what is right for each individual patient.
The trial and error aspect of it is frightening, physically challenging and takes you mentally in directions one can only understand when going through them. That’s when you have to believe. It is imperative to both mentally and physically acknowledge the challenge, face it, and be ready to fight for it as you have never fought before. I’m no superman, anyone can do it.
I went through several clinical trials. (Ugh, this means they really don’t know what the outcome will be, however, whatever it is, you will have had a hand in helping to advance that research.) We tried a strenuous STEM cell transplant that did not work, I had two hospitalized bouts of Covid, then a T-cell transplant that also did not work and quite seriously just kicked my butt. The CAR-T cell genetic re-engineering approach (they literally change your DNA—whaaat!) is absolutely the future of cancer treatment and my failed CAR-T cell treatment did not stop my oncologist, his team or me. We just kept going and after a bout of Tuberculosis (yes, you read that right and this was another period, like Covid, of isolation via quarantine). However, during my time with tuberculosis they discovered a bio-marker that they hadn't seen in me before and one which might work with the drug Keytruda…go figure... as it’s not really intended for the DLBCL cancer but it has worked miraculously for me.
There are so many lessons in this cancer journey—especially the necessity of a support team both personally and medically. Inner strength can come and go at any time in your journey and recognizing that is not easy or something you learn in a book. For me the inner strength came from my experiences during cancer and the one thing you can count on with cancer is that you will be tested and you will have to find a new strength. Undoubtedly every person has this capability and belief in them already. You just need to tap into it in any way that you are able. It is a horrible disease but it can, and I think will, be defeated in the long run. There are wins in cancer every day and one of them, like it was for me, could be just around the corner for you and your illness. #BELIEVE.
February 2025 Update
The Brian Allman DLBCL Journey: A 2025 Update
After documenting my four-year battle with Diffuse Large B Cell Lymphoma, I'm thrilled to share some long-awaited good news: I no longer have cancer! Yes, you read that right. The journey that began with a volleyball-sized tumor (which, let's be honest, gave me quite the interesting physique) and took me through R-CHOP, Polatuzumab, failed stem cell harvesting (not my finest performance), CAR T-cell therapy, and even tuberculosis (seriously, who gets TB these days?), has finally led to this moment of celebration.
My path included numerous clinical trials where I became a willing guinea pig for science. Each one represented hope, even when they didn't deliver the results we wanted. The trial-and-error nature of cancer treatment is both fascinating and terrifying—you're simultaneously a patient and a pioneer helping forge new paths for future patients. Through it all, Dr. Mei at City of Hope never ran out of options or determination, even when my body was screaming "enough already!"
As if cancer wasn't enough of a challenge, I battled COVID-19 twice during my treatments—both serious enough to land me in the hospital. The isolation of quarantine combined with the respiratory effects of COVID left me barely able to speak, much less maintain my usual optimistic outlook. Those were truly some of my darkest days, when even breathing required more energy than I could muster. Yet somehow, we pushed through.
My relationship with City of Hope and Dr. Mei continues to be one of the most important partnerships of my life. After discovering that specific biomarker during my TB diagnosis, the Keytruda treatments that followed have proven remarkably effective. What started as "no evidence of disease" has developed into sustained remission that my medical team now confidently describes as cancer-free. The drug that wasn't even intended for DLBCL became my unexpected savior. Life's funny that way, isn't it?
I couldn't have made it through this wild ride without my incredible family and support system. My wife, who waved to me through quarantine windows and brought food I couldn't taste, showed a level of patience and love that still humbles me daily. My friends who kept checking in even when I was too exhausted to respond reminded me I was never truly alone. This network of love carried me through my darkest days when my own positivity tank was running on empty.
I also owe immense gratitude to Marcia Horn at ICN (International Cancer Advocacy Network), whose guidance was nothing short of lifesaving. When the complexity of treatment options and clinical trials became overwhelming, Marcia provided clarity, connections, and compassionate advocacy that helped me navigate the medical maze. Her expertise and tireless support ensured I had access to cutting-edge options and information when I needed it most. Let me be clear: having people in your corner isn't just nice—it's absolutely essential. They lift you when you can't lift yourself, and sometimes their belief in your recovery is what keeps your own hope alive.
Physical recovery has been its own journey. From the days when walking ten steps exhausted me (not a great look for someone who used to pride himself on those long bike rides), I've progressed to cycling again and joining those park fitness classes where I'm slowly but surely becoming the resident comeback kid. My weight has normalized—goodbye skeletal 113-pound frame!—my energy continues to improve, and I've found purpose again beyond just surviving. The mental fog that once made me feel "boring" has lifted, allowing me to be the engaging, occasionally witty Brian that I've always been.
Staying positive through cancer isn't about ignoring reality or plastering on a fake smile. It's about finding those tiny moments of joy, celebrating small victories (Hey, I walked to the kitchen without help today!), and sometimes just laughing at the absurdity of it all. When you're wearing hazmat suits just to see visitors, you either find the humor or lose your mind—I chose humor whenever possible.
Looking back, the lessons of this journey seem clearer now: the importance of having an exceptional medical team that doesn't give up; the necessity of both physical and mental preparation for whatever comes; and the immeasurable value of support systems when your own strength falters. Cancer tested every aspect of my being, but it also revealed reserves of resilience I never knew I possessed.
For those still in their own cancer battles, I offer this message: treatments are advancing daily, unexpected solutions may be just around the corner, and what seems impossible today may become your reality tomorrow. The path is undeniably brutal—I wouldn't minimize that—but persistence matters more than perfection. Surround yourself with people who lift you up, find reasons to laugh, and in the words I've lived by and will continue to embrace: #BELIEVE.
Brian
Federal Tax I.D.: EIN 86-0818253